Secretion Removal Techniques in People with Spinal Cord Injury through Physiotherapy
Respiratory
complications are a leading cause of injury and mortality in people with spinal cord
injury (SCI) and are more pronounced in individuals with higher
level and complete injuries. A major contributor to respiratory illness in individuals
with SCI is secretion retention, particularly among individuals with cervical
lesions. Higher levels of SCI result in greater denervation of the ventilatory
muscles thereby decreasing both inspiratory capacity and expiratory muscle
force and resulting in an impaired cough. The figure shows the innervation
of the respiratory muscles. Cervical SCI also denervates sympathetic pathways
leading to a state of parasympathetic dominance that may increase mucus
production and contribute to airway hyper responsiveness. A diminishing cough
combined with mucus hyper secretion can overwhelm mucociliary clearance in
people with SCI.
The impact of SCI on
normal airway clearance can be exemplified by examining the sequence of a
cough. After full inspiration to total lung capacity, the glottis is closed
followed by an increasing intrathoracic pressure. Opening of the glottis is
followed by a forced, high-velocity expiratory flow, which facilitates
propagation of sputum towards the upper airway to expectorate or swallow. The
ability to inspire to a normal vital capacity (VC) is progressively hindered with
higher levels of SCI due to a greater denervation of inspiratory muscles.
Inspiring to a lower VC therefore decreases the inward recoil of the chest wall
and lungs that contributes to maximal expiratory flow. Forced expiratory flow
is further impaired in people with SCI when the injury
affects the abdominals and other expiratory muscles, such as intercostals
(thoracic roots), pectoralis, or latissimus dorsi. With high thoracic SCI the
VC might only be 30% to 50% of normal, and the cough might be weak and possibly
ineffective. Spirometric measures, such as forced vital capacity (FVC), forced
expiratory volume in 1 second, and VC, are therefore often valuable predictors
of cough strength.
Non-SCI factors such as
smoking, chronic obstructive pulmonary disease, asthma, and aging exacerbate
increased mucus secretions resulting from cervical SCI. Increasing mucus
production combined with a diminishing cough and breathing at a lower lung
volume, contributes to micro atelectasis and potential trapping of retained
secretions. Ultimately, an ineffective cough, micro atelectasis, and retained
secretions increase the risk for both pneumonia and mucus plugs, which may lead
to potential lung collapse and consolidation.
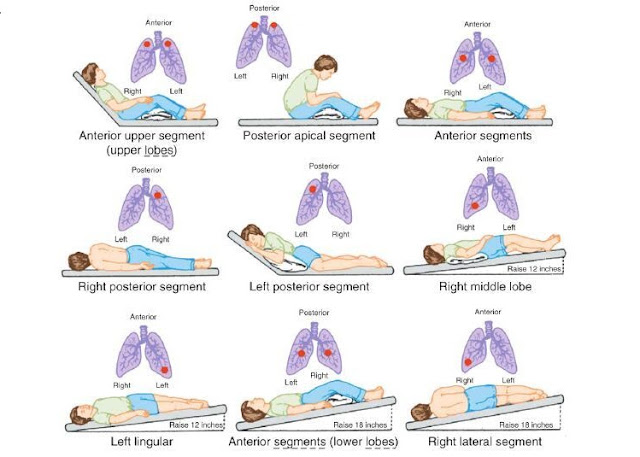
Physiotherapy
treatment to facilitate airway clearance in people with SCI has included
traditional chest physiotherapy techniques of manual percussions and vibrations
as well as postural drainage. In addition, techniques to enhance forced
expiration, including cough, have been used, such as those that improve
inspiratory capacity and strength or increase expiratory flow and strength.
Despite these physiotherapy techniques being commonly used there is a scarcity
of published evidence to support their effectiveness in SCI. This systematic
review was done to answer the question, “Do secretion removal techniques
increase airway clearance in people with chronic SCI?” Thus focused on
interventional and survey studies within the scope of physiotherapy practice,
therefore excluding pharmaceutical interventions. In addition, sequelae
associated with this acute phase, such as neurogenic pulmonary edema, unstable
fractures, or aspiration pneumonia, would complicate the interpretation of
outcomes as the result of airway clearance interventions such as percussion or
assisted cough.


Thanks for sharing. DIALYSIS SERVICES
ReplyDeleteREHABILITATION SERVICES
Thanks for sharing the technique to relieve back pain. If you are looking for the best physiotherapy center in Gurgaon, connect with DynaFisio. They provide Low Back Pain Physiotherapy in Gurgaon. Call Now: 9650091934 | 8800818568
ReplyDelete